A Third Party Administrator (TPA) performs an important position in many sectors, notably in health coverage, exactly where they work as intermediaries amongst insurance policies companies and policyholders. But just what can be a TPA? Fundamentally, a TPA is definitely an entity that manages administrative duties associated with insurance policy promises and Positive aspects on behalf of insurance policy organizations. This outsourcing lets coverage providers to emphasis more on Main functions like underwriting and plan management even though entrusting administrative processes to specialized 3rd parties.
TPAs deal with A selection of duties, generally centered around processing statements proficiently and properly. Their obligations consist of verifying declare validity, deciding coverage eligibility, and processing payments to Health care vendors. By streamlining these jobs, TPAs help minimize administrative burdens for insurers, ensuring more quickly resolution of statements and enhanced shopper satisfaction.
In the context of overall health insurance policies, TPAs are pivotal in taking care of health and fitness benefits for policyholders. They work as liaisons between insurers, healthcare suppliers, and insured persons, making certain easy communication and efficient processing of healthcare promises. This function is especially crucial in handling elaborate Health care billing processes and navigating regulatory needs.
The significance of a TPA in the Health care sector can not be overstated. They supply abilities in statements management, helping to Manage fees by negotiating favorable premiums with healthcare vendors. On top of that, TPAs improve transparency by offering in-depth studies on claims processing and expenditure, enabling insurers to help make informed decisions about protection and pricing.
Choosing a reliable TPA is paramount for insurance policy firms searching to keep up higher requirements of provider shipping. Dependable TPAs exhibit dependability in claims processing, adherence to regulatory benchmarks, and strong customer service. This reliability is essential in retaining insurance provider-shopper interactions and upholding the reputation of insurance plan providers in competitive markets.
For companies and insurers looking for nearby TPA services, factors generally consist of familiarity with regional healthcare suppliers, familiarity with community regulatory frameworks, and responsiveness to localized consumer needs. Community TPAs can supply personalised support and faster response situations, that are useful in controlling regional insurance plan functions efficiently.
In states like Minnesota and Michigan, TPAs cater to specific regional demands and regulations Tpa In Health Insurance governing coverage functions. Neighborhood TPAs in these areas are well-versed in point out-particular legislation and polices, making sure compliance and seamless integration with neighborhood Health care networks.
The top TPAs distinguish by themselves through a mix of performance, dependability, and client-centric support. Insurance plan companies generally evaluate TPAs centered on their own background in statements management, shopper fulfillment rankings, and technological capabilities. These aspects lead to choosing a TPA that aligns While using the insurance company's operational Third-party administrator MI plans and boosts Over-all service delivery.
In summary, TPAs Participate in an important role during the insurance policies ecosystem, especially in running administrative functions and enhancing support effectiveness. Their tasks span throughout different sectors, which has a Main center on healthcare where by they facilitate seamless promises processing and profit management. Deciding on the ideal TPA entails concerns of trustworthiness, experience, and alignment with community regulatory needs, guaranteeing optimal support shipping and consumer fulfillment in insurance policies functions.
 Neve Campbell Then & Now!
Neve Campbell Then & Now! Tia Carrere Then & Now!
Tia Carrere Then & Now!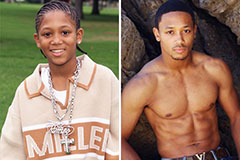 Romeo Miller Then & Now!
Romeo Miller Then & Now!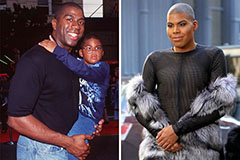 Earvin Johnson III Then & Now!
Earvin Johnson III Then & Now! Teri Hatcher Then & Now!
Teri Hatcher Then & Now!